The 12th edition provides a comprehensive overview of abnormal behavior, exploring mental health disorders, theoretical perspectives, and modern approaches to understanding human behavior and psychological well-being.
1.1 Overview of the 12th Edition
The 12th edition of Understanding Abnormal Behavior offers a detailed exploration of mental health, incorporating the latest research and clinical practices. It provides a balanced view of theoretical perspectives, including biological, psychological, and sociocultural models. The text is enriched with real-life case studies, updated statistics, and discussions on emerging trends like technology’s role in mental health. This edition emphasizes evidence-based approaches, ensuring a comprehensive understanding of abnormal behavior for students and professionals alike.
1.2 Importance of Studying Abnormal Behavior
Studying abnormal behavior is crucial for understanding mental health disorders, improving diagnosis, and developing effective treatments. It fosters empathy and reduces stigma by highlighting the complexities of psychological challenges. By examining abnormal behavior, professionals can identify risk factors, develop prevention strategies, and enhance overall well-being. This knowledge also informs public health policies and promotes a more compassionate society. Understanding these dynamics is essential for advancing mental health care and supporting individuals in need.
1.3 Key Features of the 12th Edition
The 12th edition offers updated research, expanded coverage of diverse populations, and enhanced discussion of theoretical perspectives. It includes new case studies, interactive digital tools, and streamlined organization for better comprehension. The edition emphasizes evidence-based practices, cultural sensitivity, and the latest diagnostic criteria. With a focus on student engagement, it provides robust pedagogical features like concept checks and applied scenarios. This edition is a comprehensive resource for understanding abnormal behavior in a modern, integrative context.
Theoretical Perspectives on Abnormal Behavior
The 12th edition explores biological, psychological, and sociocultural models, providing a comprehensive understanding of abnormal behavior through updated research and enhanced theoretical discussions.
2;1 Biological Model
The biological model emphasizes the role of genetic, neurological, and physiological factors in abnormal behavior. It explores how imbalances in neurotransmitters, brain structure, and hormonal systems contribute to mental disorders. This perspective is supported by advancements in neuroscience and genetic research, as highlighted in the 12th edition. By understanding the biological underpinnings, professionals can develop targeted treatments, such as medications, to address specific conditions effectively. This model provides a foundational understanding of the physical mechanisms driving mental health issues.

2.2 Psychological Model
The psychological model focuses on internal mental processes, such as thoughts, emotions, and past experiences, to explain abnormal behavior. It emphasizes how cognitive distortions, emotional regulation, and learning patterns contribute to mental disorders. This perspective highlights the role of psychological therapies, like cognitive-behavioral therapy, in addressing these issues. By understanding individual coping mechanisms and belief systems, professionals can tailor interventions to promote mental health and well-being, as discussed in the 12th edition.
2.3 Sociocultural Model
The sociocultural model emphasizes the role of cultural, social, and environmental factors in shaping abnormal behavior. It considers how societal norms, family dynamics, and cultural background influence mental health. This perspective highlights the impact of discrimination, poverty, and social inequality on psychological well-being. Understanding cultural differences in expressing distress is crucial for accurate diagnosis and effective treatment, as discussed in the 12th edition. This model advocates for culturally sensitive approaches to address diverse mental health needs.

Assessment and Diagnosis of Abnormal Behavior
Assessment involves clinical interviews, observations, and psychological testing to identify abnormal behavior patterns. Diagnosis uses standardized criteria, like DSM-5, to classify disorders accurately, ensuring effective treatment plans.
3.1 Clinical Interviews and Observations
Clinical interviews and observations are essential tools for assessing abnormal behavior. Interviews allow professionals to gather detailed information about symptoms, history, and experiences. Observations focus on behavioral patterns, emotional responses, and cognitive functioning. Together, these methods provide a comprehensive understanding of an individual’s mental state, aiding in accurate diagnosis and treatment planning. They are often the first steps in evaluating psychological distress and identifying underlying issues, ensuring a personalized approach to care.
3.2 Psychological Testing and Assessment Tools
Psychological testing and assessment tools are crucial for evaluating mental health. Standardized tests, questionnaires, and behavioral assessments provide insights into cognitive, emotional, and behavioral functioning. These tools help identify patterns, diagnose disorders, and monitor progress. They include personality inventories, neuropsychological tests, and symptom checklists. By using evidence-based measures, professionals can develop targeted interventions and improve treatment outcomes, ensuring a more accurate and comprehensive understanding of an individual’s mental health needs.
3.3 Role of DSM-5 and ICD-11 in Diagnosis
The DSM-5 and ICD-11 are essential diagnostic manuals for mental health professionals. DSM-5 provides standardized criteria for diagnosing mental disorders, while ICD-11 offers a global classification system for coding and insurance purposes. Both manuals ensure consistency in diagnosis, facilitating accurate clinical decisions and research. Updates in DSM-5 include new disorders and revised criteria, while ICD-11 introduces dimensional assessments. These tools are vital for promoting reliable diagnoses and guiding effective treatment plans, reflecting current understanding of mental health conditions.

Anxiety Disorders
Anxiety disorders are a group of mental health conditions characterized by excessive fear, worry, and anxiety that interfere with daily life. They encompass various specific disorders, each with distinct symptoms and impacts on emotional and psychological well-being.
4.1 Generalized Anxiety Disorder
Generalized Anxiety Disorder (GAD) is characterized by excessive and uncontrollable worry about various aspects of life, such as work, health, or finances. It is chronic and pervasive, often accompanied by physical symptoms like restlessness, fatigue, and sleep disturbances. Unlike other anxiety disorders, GAD is not triggered by specific situations but persists regardless of circumstances. It significantly impairs daily functioning and quality of life. Treatment typically involves psychotherapy, such as cognitive-behavioral therapy (CBT), and may include medication to manage symptoms. Early intervention is crucial for effective management.
4.2 Panic Disorder and Agoraphobia
Panic Disorder is characterized by recurrent panic attacks, which are sudden episodes of intense fear or discomfort, often accompanied by physical symptoms like rapid heartbeat and shortness of breath. These attacks can be expected or unexpected, significantly impacting daily life. Agoraphobia frequently co-occurs, involving fear of situations where escape might be difficult, leading to avoidance behaviors. Together, they create a cycle of fear and limitation, requiring targeted interventions to address both the panic symptoms and the associated avoidance behaviors effectively.
4.3 Social Anxiety Disorder
Social Anxiety Disorder involves intense fear of social situations, leading to avoidance behaviors. It is characterized by feelings of embarrassment, self-consciousness, and concern about being judged or viewed negatively by others. Physical symptoms like sweating, trembling, and difficulty speaking may occur. This disorder significantly impacts daily life, interfering with relationships and professional activities. Understanding its roots in biological, psychological, and sociocultural factors is essential for effective intervention and support, helping individuals manage their anxiety and improve their quality of life.
4.4 Specific Phobias
Specific phobias involve intense, irrational fears of particular objects or situations, such as heights, flying, or animals. These phobias trigger avoidance behaviors and significant distress. Common types include acrophobia, aviophobia, and arachnophobia. Symptoms often include panic, sweating, and heart palpitations when exposed to the feared stimulus. Treatment typically involves exposure therapy, cognitive-behavioral techniques, or relaxation methods to reduce anxiety and improve coping mechanisms, helping individuals manage their fears more effectively and enhance their quality of life.
4.5 PTSD (Post-Traumatic Stress Disorder)
PTSD develops after exposure to traumatic events, causing intrusive memories, flashbacks, and nightmares. Symptoms include heightened arousal, avoidance of triggers, and negative thoughts. Severity varies, impacting daily functioning and relationships. Treatment often involves psychotherapy, such as cognitive-behavioral therapy (CBT) or eye movement desensitization and reprocessing (EMDR), alongside medication to manage symptoms. Early intervention is crucial for recovery and improving quality of life for individuals affected by trauma.
Mood Disorders
Mood disorders involve persistent disturbances in emotional states, such as depression or mania, significantly impacting daily functioning and well-being. They include conditions like major depressive disorder and bipolar disorder.
5.1 Major Depressive Disorder
Major depressive disorder (MDD) is characterized by persistent sadness, loss of interest, and impaired functioning. It involves at least two weeks of symptoms, including changes in appetite, sleep disturbances, fatigue, feelings of worthlessness, and recurrent thoughts of death. The 12th edition highlights the importance of understanding biological and psychological factors contributing to MDD, such as neurotransmitter imbalances and stressful life events. Early diagnosis and intervention are crucial for effective management and improving quality of life for individuals affected by this condition.
5.2 Bipolar Disorder
Bipolar disorder is a mood disorder characterized by extreme mood swings, including manic or hypomanic episodes and depressive episodes. Symptoms include elevated mood, increased energy, reduced need for sleep during manic phases, and feelings of sadness, hopelessness, and fatigue during depressive phases. The 12th edition emphasizes the importance of early diagnosis, as untreated bipolar disorder can lead to significant impairment in daily functioning. Treatment often involves a combination of medication and psychotherapy to manage symptoms and improve quality of life.
5.3 Seasonal Affective Disorder
Seasonal Affective Disorder (SAD) is a type of depression linked to seasonal changes, typically occurring during fall and winter. Symptoms include lethargy, social withdrawal, and increased sleep. The 12th edition highlights that reduced sunlight disrupts serotonin and melatonin levels, contributing to SAD. Treatment options include light therapy, psychotherapy, and lifestyle adjustments. Early intervention is crucial to manage symptoms and improve quality of life during affected seasons.
Personality Disorders
Personality disorders are enduring, pervasive patterns of thought and behavior that deviate from societal norms, leading to distress and impaired functioning in personal and social contexts.

6.1 Borderline Personality Disorder
Borderline Personality Disorder (BPD) is characterized by instability in relationships, emotional dysregulation, and fear of abandonment. Individuals often exhibit impulsive behaviors and intense emotional reactivity. Symptoms include unstable self-image, difficulty maintaining relationships, and a pattern of intense, unstable relationships. Treatment typically involves psychotherapy, such as dialectical behavior therapy (DBT), which focuses on managing emotions and improving coping skills. Early intervention and consistent therapeutic support are crucial for managing symptoms and improving quality of life for those with BPD.

6.2 Narcissistic Personality Disorder
Narcissistic Personality Disorder (NPD) is characterized by an inflated sense of self-importance, a need for admiration, and a lack of empathy. Individuals with NPD often exhibit grandiose fantasies, believe they are entitled to special treatment, and may be exploitative or envious of others. They struggle with forming healthy, mutually respectful relationships due to their self-centered tendencies. Treatment for NPD is challenging, as those affected may not seek help unless they experience significant complications. Psychotherapy is the primary approach, focusing on improving empathy and interpersonal skills.
6.3 Antisocial Personality Disorder
Antisocial Personality Disorder (ASPD) is marked by a persistent disregard for others’ rights, lack of empathy, and impulsivity. Individuals with ASPD often engage in manipulative or criminal behavior, showing no remorse for their actions. Symptoms typically emerge in childhood, with behaviors like conduct disorder evolving into adult antisocial patterns. Treatment is challenging, but behavioral therapies and interventions can help manage symptoms and reduce harmful behaviors. Early intervention is crucial to improve outcomes and reduce societal impact.
Psychotic Disorders
Psychotic disorders involve severe mental disturbances, such as hallucinations and delusions, disrupting thought, perception, and behavior, significantly impairing daily functioning and reality testing abilities.
7.1 Schizophrenia
Schizophrenia is a chronic and severe mental disorder characterized by hallucinations, delusions, disorganized thinking, and negative symptoms like social withdrawal; It disrupts cognitive, emotional, and behavioral functioning, often leading to impaired daily life and relationships. The 12th edition highlights advancements in understanding its neurobiological basis, including genetic and environmental factors. Early intervention and integrated treatment approaches, such as antipsychotic medications and cognitive-behavioral therapy, are emphasized to manage symptoms and improve quality of life for individuals with schizophrenia.
7.2 Delusional Disorder
Delusional Disorder is characterized by the presence of one or more non-bizarre delusions that last for at least one month. These delusions are persistent beliefs in situations that could occur in real life, such as being followed, poisoned, or having a disease. Unlike schizophrenia, hallucinations are not prominent, and behavior is not disorganized. The disorder often causes significant emotional distress and impairment in social or occupational functioning. Treatment typically involves cognitive-behavioral therapy and antipsychotic medications to manage symptoms and improve quality of life.
Neurodevelopmental Disorders
Neurodevelopmental Disorders involve impairments in brain development, affecting learning, communication, and behavior. They emerge early in life, impacting developmental milestones and requiring specialized interventions for optimal outcomes.
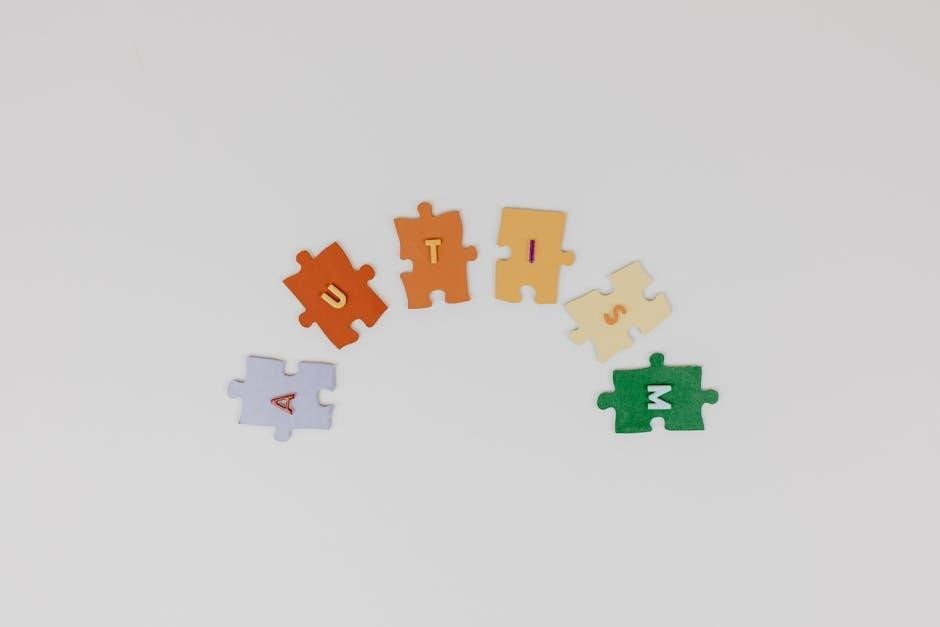
8.1 Autism Spectrum Disorder
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by challenges in social communication and interaction, alongside restricted or repetitive behaviors. Symptoms vary widely, ranging from mild to severe. Early signs often include delayed speech, social withdrawal, or repetitive movements. Diagnosis typically occurs in childhood, with interventions like Applied Behavior Analysis (ABA) therapy and supportive educational programs proving effective. Understanding ASD’s complexities is crucial for providing tailored support, fostering inclusion, and improving quality of life for individuals across the spectrum.
8.2 Attention-Deficit/Hyperactivity Disorder (ADHD)
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by symptoms of inattention, hyperactivity, and impulsivity. It often manifests in childhood, with difficulties in sustaining focus, following instructions, and controlling impulses. ADHD can persist into adulthood, impacting daily functioning and relationships. Treatment typically involves a combination of stimulant medications, behavioral therapy, and lifestyle adjustments. Early diagnosis and tailored interventions are crucial for managing symptoms and improving quality of life for individuals with ADHD;
Treatment and Intervention Strategies
Treatment and intervention strategies for abnormal behavior include biological, psychological, and alternative therapies, emphasizing a multidisciplinary approach for personalized care.
9.1 Biological Treatments
Biological treatments focus on addressing the physical aspects of abnormal behavior, often through medication. Antidepressants, antipsychotics, and mood stabilizers are commonly prescribed to regulate neurotransmitter imbalances. Additionally, therapies like electroconvulsive therapy (ECT) and transcranial magnetic stimulation (TMS) target brain activity to alleviate severe symptoms. These approaches aim to restore neurological balance, reducing symptoms of disorders such as depression, anxiety, and psychosis. Biological treatments are often combined with psychological interventions for comprehensive care.
9;2 Psychotherapy Approaches
Psychotherapy involves non-biological interventions to address abnormal behavior, focusing on cognitive, emotional, and behavioral changes. Techniques like cognitive-behavioral therapy (CBT) help individuals identify and modify negative thought patterns. Psychodynamic therapy explores past experiences to understand current behaviors. Humanistic approaches, such as person-centered therapy, emphasize self-actualization and personal growth. These methods empower individuals to develop coping strategies and improve mental well-being, often used alongside biological treatments for a holistic approach to mental health care.
9.3 Alternative and Complementary Therapies
Alternative and complementary therapies offer non-traditional approaches to treating abnormal behavior, often used alongside conventional methods. Mindfulness-based interventions, yoga, and art therapy are examples that focus on reducing stress and enhancing emotional well-being. These therapies emphasize holistic healing, addressing the mind, body, and spirit. While not replacements for evidence-based treatments, they provide additional tools for managing symptoms and improving quality of life, offering diverse options for individuals seeking complementary care.
Special Topics in Abnormal Behavior
Exploring cultural influences, legal frameworks, and societal stigma, this section examines how these factors shape understanding and treatment approaches in abnormal psychology.
10.1 The Role of Culture in Abnormal Behavior
Culture significantly influences perceptions and expressions of abnormal behavior, shaping norms, values, and beliefs about mental health. Symptoms and diagnoses vary across cultures, reflecting diverse coping mechanisms and societal expectations. Cultural background impacts how individuals express distress and interact with mental health systems, highlighting the importance of cultural competence in diagnosis and treatment. Understanding these dynamics fosters more inclusive and effective approaches to addressing mental health challenges worldwide.
10.2 Legal and Ethical Issues in Abnormal Psychology
Legal and ethical considerations are crucial in abnormal psychology, ensuring patient rights and confidentiality. Ethical principles guide psychologists in maintaining professional boundaries and informed consent. Legal issues involve involuntary commitment, mental health laws, and court-mandated treatments. Balancing individual rights with societal safety is a key challenge. Understanding these frameworks is essential for ethical practice, protecting both patients and professionals while navigating complex mental health scenarios.
10.3 The Impact of Stigma on Mental Health
Stigma surrounding mental health can lead to social isolation, discrimination, and internalized shame, discouraging individuals from seeking help. It perpetuates negative stereotypes and reinforces barriers to care. Education and awareness are crucial in reducing stigma, promoting understanding and acceptance. Addressing stigma requires challenging societal perceptions and fostering inclusive environments. By doing so, we can encourage individuals to pursue treatment without fear of judgment, ultimately improving mental health outcomes and reducing suffering.

Emerging Trends and Future Directions
Emerging trends include advancements in AI-driven diagnostics, personalized therapies, and integrative care models, with a focus on neuroscience and future research directions in technology.
11.1 Advances in Neuroscience and Genetics
Recent advancements in neuroscience and genetics have deepened our understanding of mental health, revealing biological markers and genetic risk factors. Neuroimaging techniques now provide clearer insights into brain function, while genetic studies identify predispositions to disorders. These breakthroughs are paving the way for more precise diagnoses and personalized treatments, integrating biological and psychological approaches for comprehensive care.
11.2 Technology and Digital Mental Health Tools
Digital mental health tools are revolutionizing care through AI-driven apps, virtual reality therapies, and wearable devices. These technologies enhance accessibility, offering personalized interventions and real-time monitoring. Telehealth platforms expand reach, while AI analyzes data for early disorder detection. The 12th edition highlights how these innovations bridge gaps in traditional care, fostering a more integrated and patient-centric approach to mental health support.
11.3 Integrated Care and Multidisciplinary Approaches
Integrated care emphasizes collaboration among healthcare professionals, combining medical, psychological, and social interventions. Multidisciplinary teams ensure comprehensive support, addressing the whole person. This approach fosters a patient-centered environment, improving treatment outcomes and reducing fragmentation. The 12th edition underscores the importance of such strategies in addressing complex mental health needs, promoting continuity of care and enhancing overall well-being for individuals with abnormal behavior.

The 12th edition emphasizes the importance of continued research and education in understanding abnormal behavior, fostering a deeper understanding of mental health and its complexities.
12.1 Summary of Key Concepts
The 12th edition synthesizes key concepts in understanding abnormal behavior, covering theoretical models, assessment tools, and diverse disorders. It explores biological, psychological, and sociocultural perspectives, emphasizing evidence-based practices. Disorders such as anxiety, mood, personality, psychotic, and neurodevelopmental conditions are examined in depth. The role of DSM-5 and ICD-11 in diagnosis is highlighted, along with the importance of cultural sensitivity and ethical considerations. This comprehensive approach fosters a deeper understanding of mental health, promoting effective treatment and reducing stigma.
12.2 The Importance of Continued Research and Education
Continued research and education are vital for advancing understanding of abnormal behavior, ensuring evidence-based practices, and addressing emerging mental health challenges. Ongoing studies refine diagnostic tools and therapies, while education fosters awareness and reduces stigma. By integrating new technologies and interdisciplinary approaches, future advancements can improve treatment outcomes and promote mental well-being globally. Investing in research and education ensures a compassionate and informed approach to addressing complex psychological issues.